Healing the Healers

Insights from a National Survey on WELL-Certified Strategies to Address Burnout in Healthcare
Read the full white paper below, or download a PDF copy.
Introduction
Not long ago, staff burnout in healthcare was a prominent topic in national conversations. Headlines, panel discussions, and policy memos all echoed the same concern: healthcare workers were exhausted, overwhelmed, and reached a breaking point. Recently, that urgency seems to have quieted. Has the problem been solved, or are healthcare employees adjusting to a new normal where chronic stress and mental fatigue are now part of the job?
Healthcare remains one of the most demanding industries for all professionals involved. Employees across hospitals, outpatient clinics, and specialized care still face the relentless pressure of long shifts, varying patient acuity, and the emotional burden of caring for others. In this context, staff well-being is no longer just a moral imperative but a strategic necessity for maintaining workforce stability and delivering high-quality patient care.
The WELL Building Standard references a wealth of research to link employer policies and the built environment to measurable improvements in occupant well-being. Using the framework of the Standard’s Mind feature to address cognitive and emotional behaviors, this whitepaper presents findings from a large-scale survey of approximately 745 healthcare employees. These participants include employees from diverse roles, facility types, and geographical locations to gain a holistic perspective on the current state of the industry’s mental health and resilience.
The Human Cost of Healthcare Burnout
Burnout among healthcare professionals is well-documented and has been formally recognized by the World Health Organization as an occupational phenomenon, as listed in the 11th Revision of the International Classification of Diseases (ICD- 11). The survey results from BHDP’s study confirm the prevalence: while 58% of respondents rated their well-being as “good” or “excellent,” nearly half reported feeling burned out at least two days per week, with a concerning minority still experiencing burnout five to seven days per week.
As a foundational component of overall health, an individual’s mental state can determine their ability to cope with stressors, operate productively, and make meaningful contributions to their community. Evidence shows that mental fatigue is strongly correlated with both job satisfaction and overall well-being, suggesting that environmental and organizational interventions that enhance daily enjoyment can serve as preventative measures against chronic stress. When left unaddressed, burnout can lead to increased absenteeism, turnover, and financial strain on institutions.
Well's Focus on the Mind
The WELL Building Standard’s Mind feature provides a structured, research-based framework for addressing the challenges of burnout through design, policy, and operations. Key areas include access to nature, restorative spaces, mental health resources, and organizational strategies for stress reduction. By tying survey data back to these categories, healthcare organizations can benchmark their current practices, identify gaps, and prioritize interventions.
Well V2 Mind Feature Categories
- Mental Health Promotion
- Nature and Place
- Mental Health Services
- Mental Health Education
- Stress Management
- Restorative Opportunities
- Restorative Spaces
- Restorative Programming
- Enhanced Access to Nature
- Tobacco Cessation
- Substance Use Services
Methods
Access to information about employer-offered benefits to address mental fatigue in healthcare employees remains limited or restricted behind subscription models. A survey was developed to target what the WELL Building Standard refers to as regular occupants: individuals who spend at least 30 hours per month across at least 5 days in any given building. Questions were designed around the WELL Mind feature requirements of each focus category, and responses were analyzed using valid percent to capture the most accurate picture. Correlation analysis (phi coefficient) was applied to detect the effectiveness of established programs, while demographic cross-tabs explored role, tenure, and location differences.

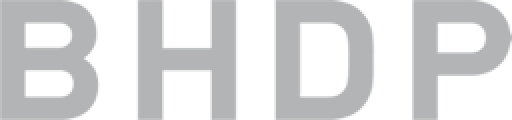
The survey captured responses from 745 healthcare employees across many roles, including Registered Nurses (18.6%), Nursing Assistants/Patient Care Technicians (8.9%), Behavioral Health professionals (10.1%), Administrative/Clerical staff (7.8%), Physicians (7.3%), Therapists (7.7%), and others. Facility types ranged from general acute-care hospitals (22.2%) and academic medical centers (13.6%) to nursing homes (6.5%) and specialty hospitals (11.8%). Respondents were distributed across urban (43.6%), suburban (40.3%), and rural (16.1%) settings.
Insights from the Data
1. Connection to Nature and Community
Insight Description: Environments that combine references to nature and community support a sense of belonging and emotional ease.
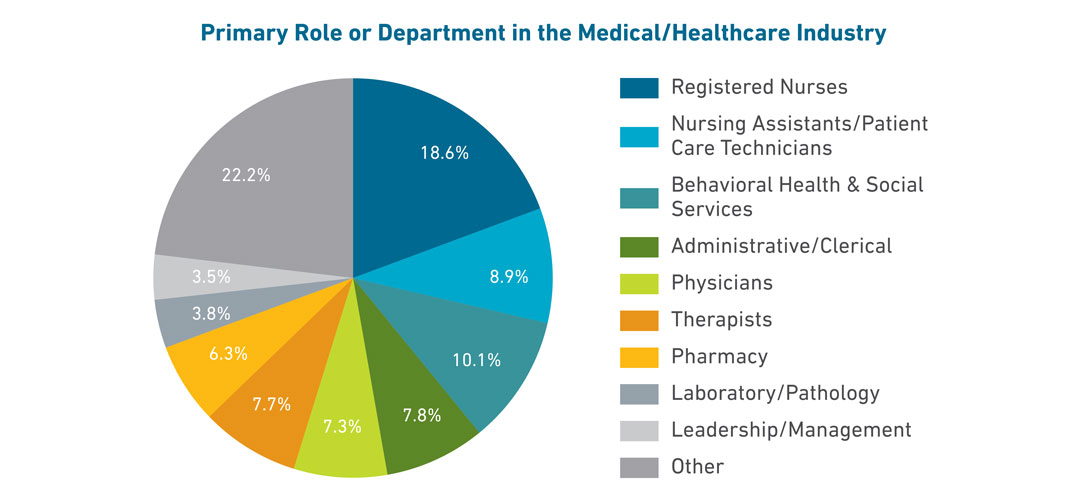
69% reported some form of access to nature.
The degree of employer-provided access employees have to outdoor spaces
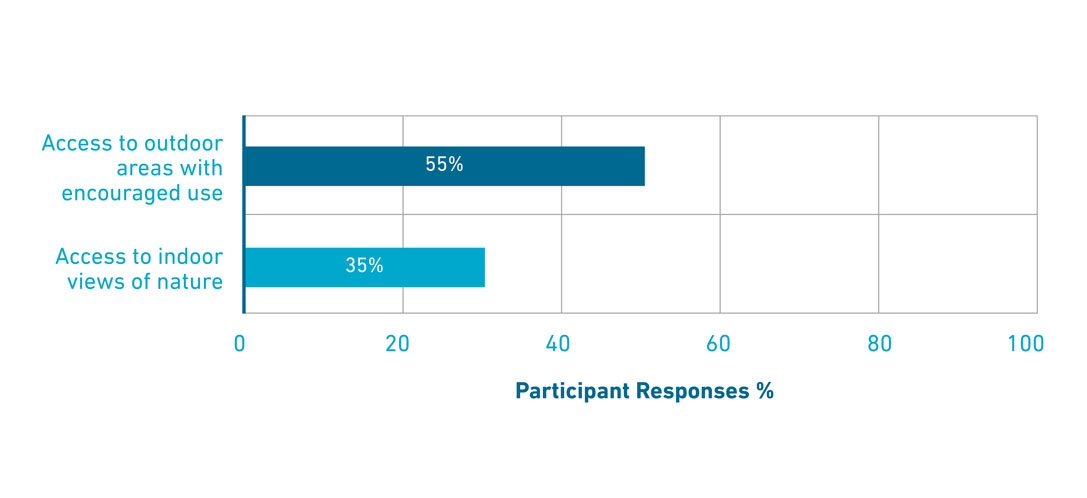
61% reported their workplace integrates representational elements of nature through art, materials, patterns, or cultural identity cues.
Responses indicating the degree of Integration of nature through art, materials, patterns, or cultural identity elements in the Workplace

Interpretation: Outdoor access remains the dominant restorative driver, while indoor, representational elements of nature and community are strong restorative drivers but less consistently delivered. Importantly, employees who noticed outdoor access also tended to notice indoor elements either directly or through representation.
2. Recovery and Restoration
Insight Description: Policies that limit long or consecutive shifts and support microbreaks help enable mental recovery and sustained well-being.
Type of support employers provide for recovery and restoration from work
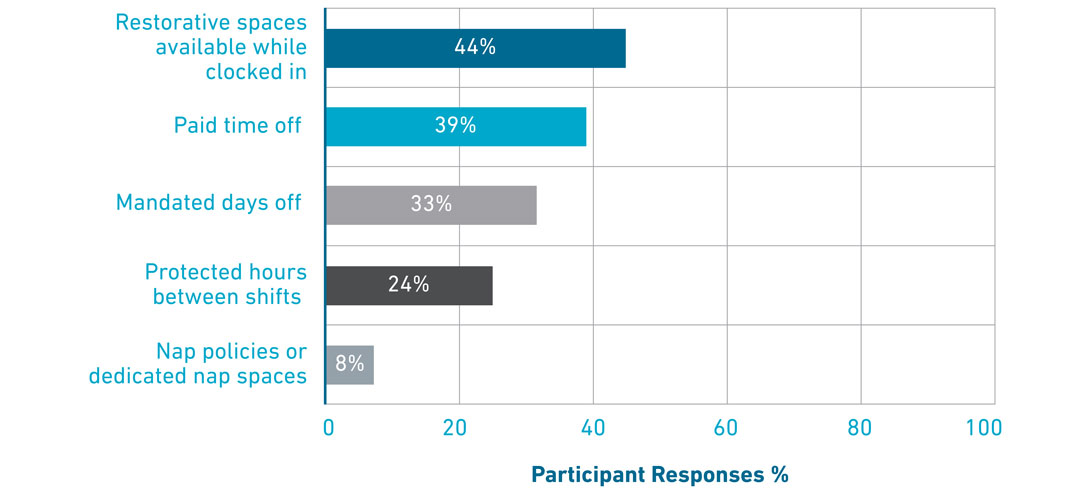
69% reported access to structured recovery benefits.
- Most commonly paid time off (39%), mandated days off (33%), or protected hours between shifts (24%).
- Only 8% reported nap policies or dedicated nap spaces.
- 44% reported restorative spaces available while clocked in, but awareness gaps were significant (21% answered “I don’t know”).

Interpretation: Macro-scale time-off structures dominate recovery supports, but on-shift micro-recovery spaces are either not offered, underrecognized, or underutilized.
3. Wellness Programming
Insight Description: Mindfulness-based restorative offerings combined with a supportive infrastructure promote emotional balance and mental clarity.
Type of mindful based restorative offerings employers provide for recovery and restoration from work
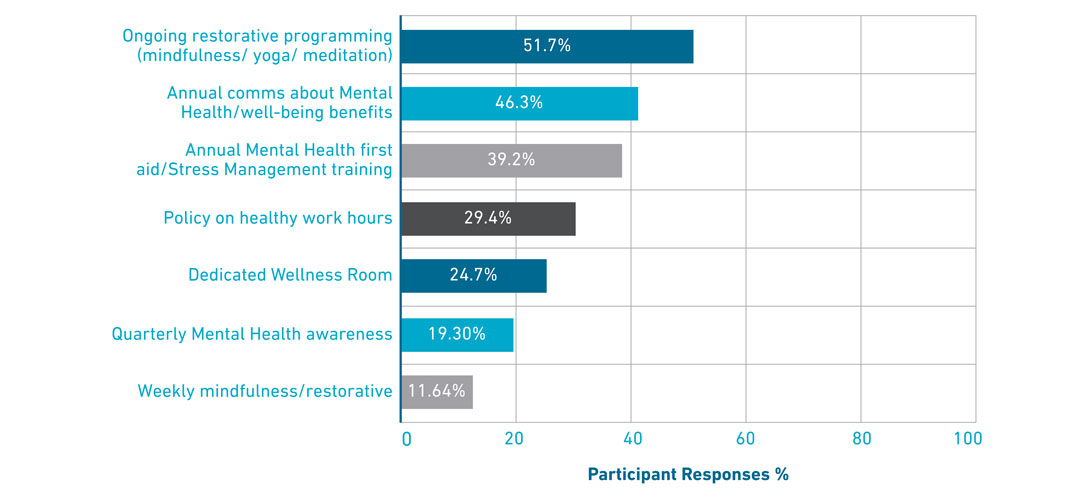
- 42% reported ongoing restorative programs (e.g., mindfulness, yoga).
- 74% reported well-being promotion through annual communications, training, or wellness rooms.
- Weekly programming was rare (12%).

Interpretation: Institutions tend to prioritize annual events and communications over frequent, small-scale restorative programs. Yet the survey indicates that these micro- programs are strongly correlated with perceived benefit utilization.
4. Mental Health and Stress Management
Insight Description: Proactive strategies like staff surveys, mental health screenings, and manager training help organizations identify stressors and support employee well-being.
Strategies employers use to identify stressors and support employee wellbeing
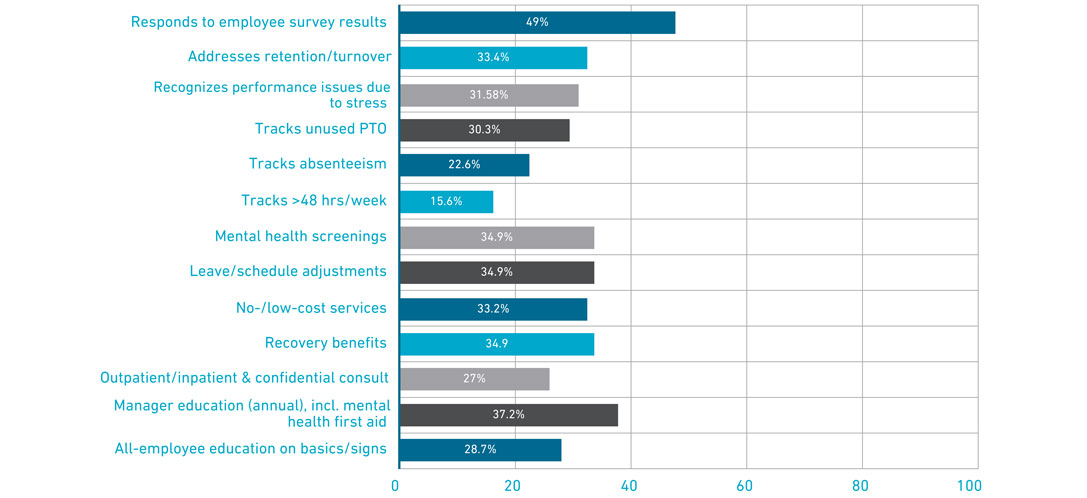
- 69% reported their employer assesses and acts on workplace stress, primarily through staff surveys (48%) and turnover monitoring (33%).
- 69% also reported access to employee programs and mental health screenings.
- Training for managers on mental health was recognized by 48%, with high uncertainty (32% answered “I don’t know”).

Interpretation: While policy frameworks are relatively common, awareness remains uneven. Staff often do not recognize available programs, highlighting a policy-to-practice gap.
5. Substance Use and Tobacco Cessation
Insight Description: Clear policies and supportive programs empower employees to address drug and alcohol use to promote better workplace behaviors.
Policies and supportive programs employers provide to address drug and alcohol use
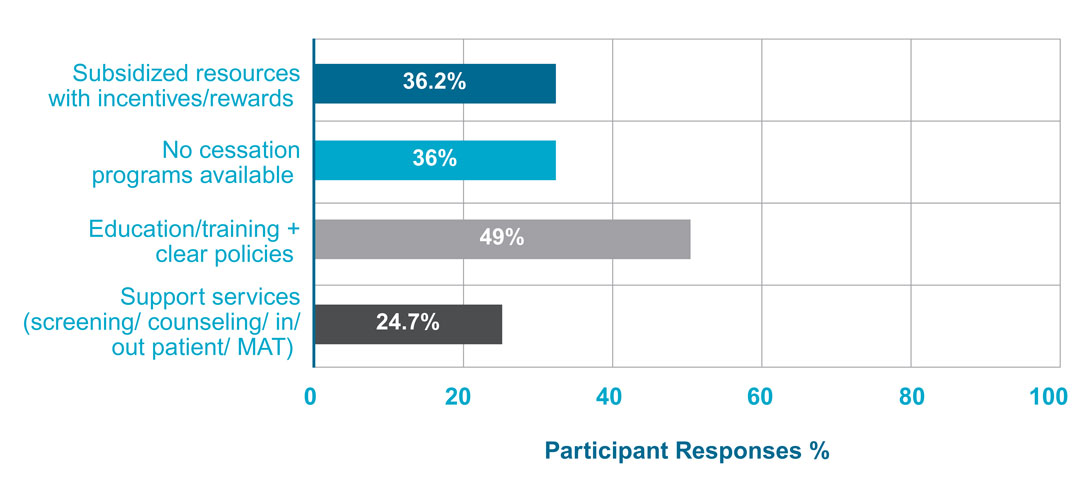
- 66% reported tobacco cessation programs, though nearly 25% said they were unaware of such programs.
- 56% reported workplace policies around alcohol and substance use, with support services less frequently visible (25%).

Interpretation: These benefits exist but are poorly communicated, indicating that the location and design of communication materials (e.g., analog and digital posters, fliers, and videos) about such cessation programs is a critical intervention point.
6. Utilization and Awareness of Benefits vs. Job Enjoyment, Well-Being, and Burnout
Insight Description: Employee awareness and engagement with available benefits influence overall job experience and sense of mental fatigue.
Utilization and Awareness:
- Only 9% said they take advantage of “many” benefits, compared to 62% who use “some” and 28% who use “none.”
- Awareness is a decisive factor: respondents who used “many” benefits had an average “I don’t know” rate of only 4.6%, compared to 22.1% among those who used none.
The top five highest rates of “I don’t know” responses came from the following questions:
- 27.1% - Training for employees on managing mental health
- 25.4% - Drug and alcohol policy/support services
- 23.0% - Tobacco cessation support
- 17.3% - Ongoing Restorative Programming Offered
- 16.5% - Restorative Spaces Available On-Site
Job Employment, Well-Being, and Burnout:
- 58% of respondents rated well-being as good or excellent.
- Respondents with high job satisfaction were strongly associated with positive well-being.

- Respondents who are less likely to enjoy their job correlated with burnout.

- Burnout was most common at 1–2 days per week, but 20% of respondents reported burnout five or more days per week.
Interpretation: Utilization follows visibility. Employees who are aware of and utilize programs that address mental fatigue are more likely to report feeling less burned out than their counterparts. Job enjoyment appears to function as a leading indicator of staff well-being, tightly linked to restorative design and supportive benefits.
Perception of Well-Being VS. Utilization and Awareness Table
A perceived provision metric is a subjective measure of how individuals experience or feel about the availability of a resource. Unlike an objective metric that calculates the actual supply of a resource, a perceived provision metric is based on human perception and lived experience.
Numerical values were assigned to each response based upon the respondents’ rated well-being to calculate percentages. The perceived provision (pp) metric indicates how much more likely a staff member was to report positive well-being compared to utilization and awareness of employer policy by subtracting the percentage of negative ratings from positive ratings. Listed below are the top 8 themes ranked in order of significance of the gap between “taking advantage = many” respondents and “none” respondents in perceiving provision of well-being:
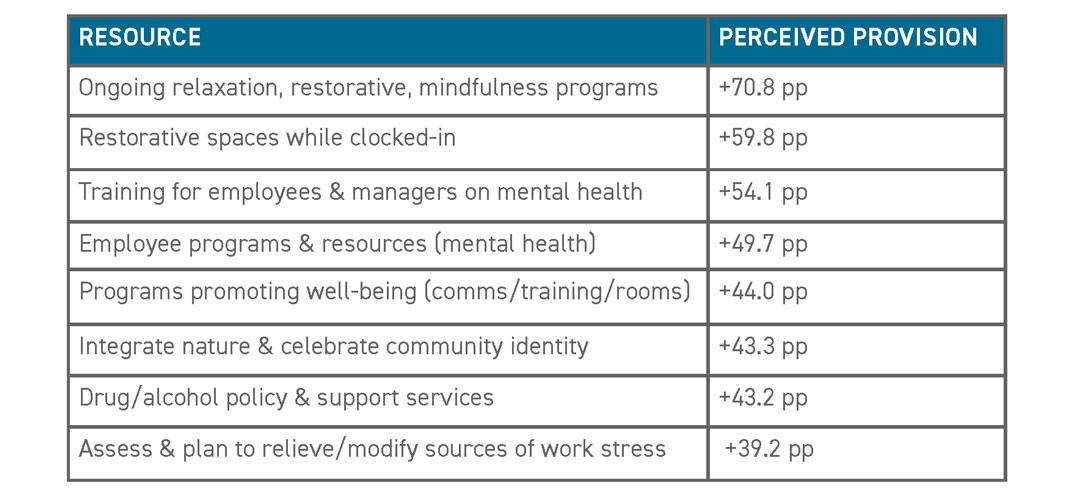
Interpretation: Providing and communicating employer benefits surrounding relaxation programs, on-the-clock restorative opportunities, and mental health training will have the highest impact on improving staff well-being and self-depiction of burnout.
Design Implications
1. Design with Nature as a System
- Combine outdoor access, indoor views, cultural art, and natural materials into a coherent building narrative.
- Integrate restorative spaces with visible programming to reinforce ecological coherence.
2. Prioritize Visibility of Recovery Spaces
- Label restorative rooms clearly, add digital booking displays, and place cues in circulation paths.
- Design decompression spaces near nurse stations, breakrooms, and dedicated staff areas for short, predictable recovery opportunities.
- Micro-recovery assets such as quiet rooms, breakrooms along the exterior, reclining chairs, and tunable lighting, can substitute where nap rooms are infeasible.
- Pair micro-recovery with end-of-shift programs (stretching, mindfulness) to target the 2–3 day burnout plateau.
3. Create Policy and Space Initiatives
- Strong correlations between restorative spaces and ongoing programming suggest that they should be planned together.
- For example, a wellness room with posted weekly mindfulness sessions and QR code access to resources.
- Determine wellness initiatives that align with staff organizational goals and provide dedicated spaces to support these initiatives.
- Foster the importance of thoughtfully designed, dedicated staff areas, giving them the same priority as patient areas.
4. Awareness Infrastructure
- Communication design should be treated as infrastructure: signage, QR codes, and stack maps.
- Reduce “I don’t know” responses as a KPI for design and policy interventions.
Implications for Healthcare Employers
Integration of WELL Mind features and employee awareness of wellbeing policies will drive success when implementing strategies to address burnout.
1. Policy-to-Practice Funnel
- Leadership teams should lead the initiatives for wellness and health policies while ensuring follow-through amongst executives, i.e. “lead by example”.
2. Wellness and Health Policies Must Be Matched with Easily Accessible and Anonymous Pathways
Examples include QR codes in staff-only areas, manager talking points during shift huddles, etc. Tailor communication by role and tenure.
- Long-tenured employees reported higher awareness of benefits, likely due to eligibility or familiarity.
- New hires and rural locations require targeted awareness campaigns.
- Pair annual campaigns with more frequent “micro-drops” of information, such as digital reminders, posters, and staff huddle scripts.
- Consider delivery methods (emails, text messaging, manager meetings, allcalls) and frequency.
3. Measure Visibility and Treat Job Enjoyment as a KPI
- Programs are only as valuable as employees’ awareness of them. Include ongoing tracking of awareness in employee satisfaction surveys. “I don’t know” should be tracked as a failure point.
- Treat job enjoyment as a KPI. Since enjoyment correlates with both wellbeing and burnout, institutions should adopt it as a leading indicator of staff health.
Conclusion
The survey results underscore that healthcare organizations are making progress in supporting mental fatigue but still face critical gaps in awareness, communication, and integration. Though it appears that burnout in healthcare employees may be improving, provision without visibility is ineffective when discussing solutions to solve the problem. The data demonstrates that holistic strategies to combine restorative spaces, biophilic interventions, and ongoing policy programming are most strongly associated with perceived utilization and staff well-being.
For healthcare leaders, the opportunity lies in treating communication and awareness as design challenges equal to policy creation. By aligning design, operations, and communication, organizations can reduce burnout, improve well-being, and ultimately enhance patient care through a healthier, more resilient workforce.
References
- International WELL Building Institute, PBC. WELL Building Standard. Version 2., 2020.
- Well-being in Healthcare Survey
- World Health Organization. Protecting health and care workers’ mental health and well-being: Technical Consultation Meeting. 25 Apr. 2024, WHO, https://www.who.int/news/item/25-04-2024- 202404_protecthw_mentalhealth
Author
Content Type
White Paper
Date
January 07, 2026
Market
Practice
Topic
Healthcare Design